|
Management of Chronic Kidney Disease in Cats Martha Cannon BA VetMB DSAM(Fel) RCVS Specialist in Feline Medicine Cats with chronic kidney disease (CKD) are seen every week in veterinary practices across the country. The third part of this special focus on chronic disease in cats discusses management of CKD in cats. Martha Cannon from The Oxford Cat Clinic reviews the current management options in cats with CKD. Chronic kidney disease (CKD) is a common disorder of cats, particularly those in middle to old age, and is a major cause of illness and death in the pet cat population. Previous articles in this series have covered the common causes of CKD in cats and have reviewed the clinically significant aspects of its pathophysiology. This article will look at current recommendations for the management of cats with CKD from the early stages through to more advanced stages of the disease. Consequences of CKD The kidneys have an important role in a wide range of physiological functions, any or all of which may be deranged once kidney disease is established. The consequences of these derangements contribute to the clinical signs that the cat suffers. However, in many cases they are themselves damaging to the kidneys, contributing to further deterioration in renal function and an inevitable progression of disease. In the early stages of disease (IRIS Stages 1 and 2), clinical signs of kidney disease may be minimal but identification and effective management of some of the metabolic consequences of CKD can have a significant effect in slowing down the progression of disease. In the later stages (IRIS Stages 3 and 4), azotaemia becomes more severe and clinical signs become apparent: nausea and uraemic gastritis cause diminished appetite and polyuria exceeds polydipsia causing dehydration. Weight loss due to muscle catabolism contributes to the azotaemia and promotes further deterioration in both wellbeing and renal function. Maintaining fluid balance and appetite, and diminishing nausea become important aims of management and contribute to both quality of life and longevity. Management of Early CKD to Limit the Progression of Disease If the presence of CKD can be identified early in its course, while the cat remains relatively asymptomatic, much may be done to limit the progression of disease and maintain good quality of life. Early diagnosis requires regular screening of older cats, particularly with regard to their urine specific gravity (SG) and serum creatinine levels. A decline in urine SG to below 1.030 and an upward trend in serum creatinine, even if it remains within the reference range, may be indications of kidney disease. If these changes are consistent over several months, and if no other contributing cause such as hyperthyroidism can be identified, CKD should be suspected. Once CKD is identified, further investigations will identify the range of metabolic consequences currently present, allowing a treatment plan to be tailored to the specific needs of the individual cat. Important factors that must be identified and treated include:
Healthy cats have very low levels of protein in their urine, but proteinuria can develop as a consequence of CKD. The presence of significant proteinuria also appears to be a predictor of more rapid progression of CKD and of poorer survival time in affected cats (Elliot and Syme, 2006). Screening all cats with CKD for the presence of renal proteinuria is important, and treatment is recommended if the urine protein:creatinine ratio (UP:C) is persistently elevated in the absence of evidence of urinary tract infection or lower urinary tract disease.
ACE inhibitors have been the only available treatment for renal proteinuria and are effective in reducing the UP:C in most cases. However, they must be used with care in cats with advanced CKD as they may reduce glomerular filtration rate (GFR), which will promote worsening azotaemia (see Box 1). Serum Phosphate /Hyperphosphataemia Renal secondary hyperparathyroidism is a common consequence of CKD and is itself a significant cause of progression of renal disease. To adequately control parathyroid hormone (PTH) secretion, serum phosphate must be maintained within the lower half of the reference range. Currently recommended targets for serum phosphate are:
Controlling hyperphosphataemia is a long-term strategy, and a staged process:
Changes should be introduced gradually: take 2–3 weeks to alter the diet and, if using phosphate binders, introduce them slowly and increase to the recommended starting dose over 2–3 weeks. Restricting phosphate intake causes hypercalcaemia in a small proportion of cats. Serum calcium should be monitored and if hypercalcaemia occurs it will be necessary to allow a higher serum phosphate level in order to correct the hypercalcaemia. Hypertension
Systemic hypertension is a common complication of feline CKD, which may easily go unrecognised (see Figure 1). Untreated it can cause significant damage (ocular bleeding, retinal detachment, intra-cranial bleeding, cardiovascular disease), and will also contribute to the progression of kidney disease. Figure 1: Blood pressure measurement in a cat with chronic kidney disease. In cats with CKD, hypertension is defined according to the “risk of causing end organ damage”: a continuum rather than “normal” versus “high”.
Anti-hypertensive treatment is recommended if there are clinical signs of hypertension, or if blood pressure is persistently >160 mmHg. Initial treatment is with amlodipine (0.625–1.25 mg once daily), though amlodipine is not licensed in cats, with additional use of an ACE inhibitor if:*
Hypokalaemia Cats with CKD may also develop hypokalaemia, probably due to a combination of increased urinary potassium excretion and the presence of metabolic acidosis. Hypokalaemia causes a myopathy that is seen initially as a stiff, stilted gait (sometimes mistaken for arthritis in elderly cats) and a poor hair coat. In more severe cases there is marked muscle weakness causing ventroflexion of the neck. Serum potassium should be maintained at or above 3.5 mmol/l. Renal diets are moderately potassium supplemented and will help to prevent hypokalaemia. Additional oral potassium supplementation may also be required. Urinary Tract Infections Urinary tract infections (UTIs) are rare in healthy cats but are a common complication of CKD, especially in female cats. These infections are usually asymptomatic and will not be identified unless urinalysis is routinely performed as part of the regular screening of cats with CKD (see Figure 2). Treatment of UTIs in cats with CKD should be aggressive to prevent or eliminate 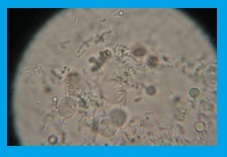 pyelonephritis; a 4–6 week course of antibiotic treatment is required, and the choice of antibiotic should be based on culture and sensitivity results. Urine sediment should be clear of signs of infection within 4 days of starting treatment, and repeat urinalysis and culture is indicated 10 days after the end of the course of treatment to ensure that the UTI has fully resolved. pyelonephritis; a 4–6 week course of antibiotic treatment is required, and the choice of antibiotic should be based on culture and sensitivity results. Urine sediment should be clear of signs of infection within 4 days of starting treatment, and repeat urinalysis and culture is indicated 10 days after the end of the course of treatment to ensure that the UTI has fully resolved.
Figure 2: Microscopic evaluation of a urine sample showing evidence of bacterial rods indicative of a urinary tract infection (UTI). Management of Advanced CKD to Moderate Azotaemia Preventing Dehydration Inadequate fluid intake causing sub-clinical dehydration is a common problem in cats with CKD. The approach to management will depend on the severity of the dehydration:
Figure 3: A cat with chronic kidney disease and clinical evidence of dehydration receiving intravenous fluids. Cats that fail to maintain adequate fluid intake over the longer term will tend to suffer cycles of deteriorating appetite and decompensation of clinical signs requiring admission to the veterinary practice for intravenous fluid treatment. This can be avoided by:
Box 1: Use of angiotensin converting enzyme inhibitors in CKD Effect on Progression of Kidney Disease Angiotensin converting enzyme (ACE) inhibitors reduce vasoconstriction and promote sodium and water excretion. They also appear to have renoprotective effects in some species (humans and rats) by reducing glomerular hypertension, reducing proteinuria and possibly by additional effects on the glomerular basement membrane. In humans it appears that the use of ACE inhibitors early in the course of CKD may slow down the progression of tubulointerstitial injury, but studies into this potential effect in cats are currently lacking. Use in Cats with Proteinuria In a study of 61 cats with naturally occurring CKD (Mizutani et al. 2006), use of benazepril significantly reduced the level of proteinuria in treated cats. However, while there also appeared to be a reduced rate of progression from IRIS Stage 2 and 3 CKD to Stage 4 CKD, there was no significant effect on longevity. Similarly in a study of 153 cats (King et al. 2006) proteinuric cats treated with benazepril showed a reduction in the level of proteinuria and some improvement in subjective markers of quality of life such as improved appetite, but there was no significant effect on longevity. It appears then that administration of an ACE inhibitor lessens proteinuria in cats with CKD and proteinuria is recognised as a poor prognostic indicator for cats with CKD. However it has yet to be established whether reduction of proteinuria with use of ACE inhibitors improves the long-term prognosis in these cats (Elliot and Syme, 2006). Use in Cats with Non-Proteinuric CKD The role of ACE inhibitors in non-proteinuric, non-hypertensive cats with CKD is less clear. Extrapolation from human medicine would suggest that their use is indicated early in the course of disease, but studies in cats have not to date shown evidence of beneficial effect. Further Considerations with ACE Inhibitor Use in Cats ACE inhibitors reduce glomerular hypertension by causing more profound vasodilation in the efferent glomerular arteriole than in the afferent arteriole. In studies on cats with surgically induced kidney disease (Brown et al. 2001, King et al. 2002), use of an ACE inhibitor reduced glomerular intracapillary pressure and increased glomerular filtration rate (GFR). In some patients however, serum creatinine concentrations can increase following administration of ACE inhibitors. This is normally caused by a reduction in glomerular hypertension and not normally clinically significant, but use of ACE inhibitors in cats with acute renal failure is contraindicated. In all cases, renal parameters should be monitored following initiation of treatment and use of an ACE inhibitor should be stopped if the patient goes into acute renal failure. Maintaining Adequate Food Intake Feeding a low protein, low phosphate diet is an important tool in the management of CKD (see Box 2). However, at the time of first diagnosis, cats with advanced CKD are likely to be inappetent, uraemic and nauseated with poor appetite and little inclination to accept a new diet. In these cases, dietary change is not the first priority in treatment and should be avoided until the cat’s appetite has improved. Offering a new diet to a cat that is suffering nausea and inappetence may induce a learned food aversion to that diet. Treatment to reduce azotaemia and improve wellbeing should be allowed to take effect before trying to change the cat’s diet. In the meantime offering small amounts of the cat’s favourite foods and treats will help to encourage food intake. Using foods with a higher fat content or adding flavourings (e.g. tuna juice, chicken broth) may help.
Box 2: Nutritional Management of CKD Dietary modification is essential in the management of CKD. Feeding a low protein, low phosphate diet improves the cat’s wellbeing, reduces the speed of clinical deterioration, and increases life span by delaying the decision for euthanasia. In a study of cats with naturally occurring CKD, cats fed an appropriate “renal diet” survived an average of 633 days compared to 264 days for cats fed a normal diet (Elliott et al. 2000). Appropriate diets have restricted levels of protein, phosphorous and sodium, and are supplemented with potassium and water soluble vitamins. In general, canned diets are preferred to equivalent dry diets as they have significantly higher water content and provide calories as fats rather than carbohydrates. Excessive protein restriction can have serious negative consequences, leading to weight loss, hypoalbuminaemia, anaemia and metabolic acidosis. Using a commercial “renal” diet and ensuring adequate food intake avoids this. Having recommended a diet change, it is essential to ensure that food intake is adequate for the cat’s needs. Owners must introduce the new food gradually, over a 2–3 week period, monitoring their cat’s food intake to ensure that it is eating the new food before the familiar food is withdrawn. The cat should also be re-examined and weighed regularly so that any weight loss can be identified early. NB: If a cat with CKD will not eat an appropriate “renal” diet then the diet must be changed to an alternative food that the cat will eat. Any food is better than no food: body protein catabolism will have more serious adverse effects than almost any diet.
Management of Nausea and Vomiting Many cats with CKD suffer nausea and/or vomiting due to uraemia and uraemic gastritis, and this will contribute significantly to poor appetite even if the cat is not actively vomiting. In addition to using intravenous or subcutaneous fluids to minimise azotaemia, long-term use of H2 receptor antagonists and short-term use of anti-emetics may help. Management of Anaemia Anaemia is a common complication of advanced CKD. The anaemia is usually non-regenerative, slowly progressive, and difficult to reverse:
This article was kindly provided by Boehringer Ingelheim, makers of Semintra®:
References Brown SA, Brown CA, Jacobs G, Stiles J, Hendi RS, Wilson S. Effects of the angiotensin converting enzyme inhibitor benazepril in cats with induced renal insufficiency. Am J Vet Res 2001; 62: 375–83. Elliott J, Rawlings JM, Markwell PJ and Barber PJ. Survival of cats with naturally occurring chronic renal failure: Effect of dietary management. J Small Anim Pract 2000; 41: 235-242. Elliott J, Syme HM. Proteinuria in chronic kidney disease in cats — prognostic marker or therapeutic target? J Vet Intern Med 2006; 20: 1052–53. King JN, Strehlau G, Wernsing J, Brown SA. Effect of renal insufficiency on the pharmacokinetics and pharmacodynamics of benazepril in cats. J Vet Pharmacol Ther 2002; 25: 371–78. King JN, Gunn-Moore DA, Tasker S, Gleadhill A, Stehlau G, BENRIC Study Group. Tolerability and efficacy of benazepril in cats with chronic kidney disease. J Vet Intern Med 2006; 20: 1054–64. Mizutani H, Koyama H, Watanabe T, et al. Evaluation of the clinical efficacy of benazepril in the treatment of chronic renal insufficiency in cats. J Vet Intern Med 2006; 20: 1074–79.
*Not licensed for management of hypertension in cats This article was previously published in 2014 See the complete article |
Advertise VET Jobs for
FREE Practice Website Deal
Get the VetBoss Deal for a competitive edge on everyday products Get The VetBoss Deal for
FREE CENTRIFUGE & Great Rates
SAVE 20% JUST FOR VetBoss Members
Get the VetBoss Deal for a competitive edge on everyday products
HAPPY NEW YEAR wishing you a happy and prosperous 2014
Get The VetBoss Deal for a FREE iPad Air
Get The VetBoss Deal with THE BEST Deal on Pestigon (fipronil)
One of the many benefits of being a VetBoss member is access to exclusive deals on a range of everyday products...
This month we're offering VetBoss members a FANTASTIC deal on Pestigon. Pestigon contains Fipronil and is available in a range of practical sizes for dogs and cats. Don't let your flea product sales slip away - boost your margins. Buy any 2 packs and get 3 packs FREE!
CLICK HERE for more details
To take advantage of this cracking deal please contact your Norbrook representative and remember to quote VetBoss.co.uk as this offer is exclusively available to VetBoss members and THE BEST offer available.
Thank you to Norbrook for offering this great deal for VetBoss members
Get a FREE iPad Air on all orders over £7,000! Thinking of going digital or do you desperately need a new ultraound scanner, or would you just really like a shiny, new iPad Air? Well we've teamed up with our friends at BCF Technology to bring you THE BEST DEAL on all of their kit!
Simply quote VetBoss.co.uk when you place an order with BCF Technology and get a FREE iPad Air when you spend over £7,000.
As a vet in practice I have expereinced first hand how valuable having a user friendly system can be but should you need some convincing BCF Technology have also developed a cost calculator to help you see how much additional revenue you could generate. Remember to quote
|
|
|
Come back soon - there'll be something shortly! |